Hancock Medical
A world-class medical partner, a vital community foundation, a state-of-the-art facility and hometown heart make this hospital a vital resource.
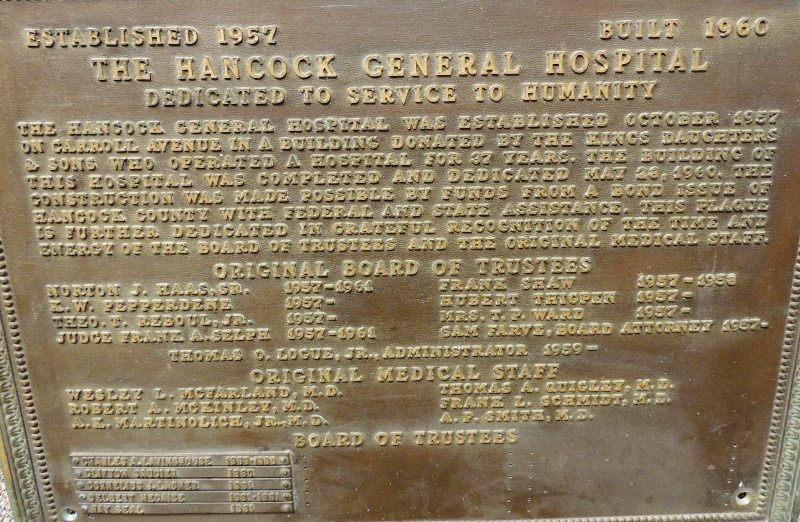
In 1987, the current Drinkwater Boulevard acute care facility opened and the hospital became fully accredited by the Joint Commission on Accreditation of Healthcare Organizations.
Although the hospital suffered $26 million in damages during Hurricane Katrina, a heroic group of employees and physicians remained and helped put lives, homes, and the hospital back together. Like any fine hospital, expansion and programs to update procedures and equipment are ongoing, with each technological advance in health care. For instance, consider the new Telestroke System. When a patient arrives at the emergency department at Hancock Medical with the symptoms of a stroke, a computer with an advanced webcam will be brought to the bedside where the clinical team will connect with a vascular neurologist on call at Ochsner’s mother-ship hospital in New Orleans. The neurologist, patient and clinical team at Hancock Medical can see and speak to each other throughout the consult. The physician examines the patient and reviews the CT scan of the patient’s head, providing guidance on advanced treatments within minutes. Bay St. Louis resident Roy Herron was the beneficiary of the new system. One morning Mr. Herron could not hold a cup of coffee in his right hand and started feeling a numbness on his right side. Concerned, he drove himself to the hospital.
After quickly being assessed on screen by the neurologist back at Ochsner Medical Center in New Orleans through the Telestroke system at Hancock Medical, Mr. Herron was assessed as having a stroke. ER Physician Dr. Laurie Patterson was instructed to administer Activase, the clot-busting drug used to treat a stroke in its early stages. Activase is used for improving neurological recovery and reducing the incidence of disability. It needs to be administered with three hours after the onset of stroke symptoms.
In many cases, Telestroke consultation will allow patients to stay at Hancock Medical. In more complicated cases, like this one involving Mr. Herron, the patient is transferred to Ochsner in New Orleans for more specialized treatment. Telestroke helps save more lives even with advanced cases because the neurologist will have already met and started treating the patient. Herron believes that the new system – and the staff – saved his life. “I wouldn’t be here today if not for the efficiency of Hancock Medical and the coordination with Ochsner,” he said. His emergency room physician at Hancock Medical that day, Dr. Laurie Patterson, believes that this case is one of many each week that prove how local hospitals help save lives. “In the case of Mr. Herron,” she said, “he got here quickly, got the meds he needed here in our Emergency Department and then was transferred to Ochsner in a timely manner.”
The Foundation
The Telestroke Program is made possible by a grant obtained by Ochsner and operating expenses paid by the Hancock Medical Foundation. The Hancock Medical Foundation, a 501(c)3, raises money to help purchase needed medical equipment for the hospital. Foundation funds also can help with services like Telestroke or mammography assistance.
The very active foundation makes many things like these possible for Hancock Medical:
The Hancock Medical Foundation Board includes Myron Labat (President), Ellis Cuevas, Theresa Bourgeois, Herb Dubuisson Sr., Suzi Lee, Bob McBee, Hank Wheeler, Jeanie Moran, Marilyn Sefton and Ron Hyman. They work closely with the Board of Trustees and hospital administration members – like Virginia Kenny. Currently Chief Nursing Officer, she’s served in many nursing roles in the hospital since 1982.
The CEO 
The foundation also works closely with Hancock Medical CEO Alan Hodges. Hodges brings more than 28 years of healthcare experience to the table, most recently serving as the Chief Operating Officer for Ochsner Health System’s North Shore Region.
Hodges says that he’s excited to help lead Hancock Medical into the future as it delivers quality health care to the residents of Hancock County. “Our core mission is to be the health resource for Hancock County and it speaks well of our facility that 80 percent of all of our inpatients and outpatients live right here in Hancock County,” Hodges says. “I’m proud of how friendly and dedicated our staff is to our patients and our community, and I’m proud of the quality health care that we’re providing.” That quality has been most recently recognized with Hancock Medical named one of eight hospitals in the state to be rewarded with an increase in Medicare reimbursement, a direct correlation to the quality of health care services it is providing patients. And in 2015, County Health Rankings by the Robert Wood Johnson Foundation Program rank Hancock County 7th for health outcomes among the 82 counties in the state. This study reflects the success of Hancock Medical and Hancock County in providing resources toward the overall health of its citizens. According to Hodges, the Hancock Medical and Oschner team add up to two things: Hometown heart and world-class care. Comments are closed.
|
Categories
All
Archives
July 2024
|
Shoofly Magazine Partners
Our Shoofly Partners are local businesses and organizations who share our mission to enrich community life in Bay St. Louis, Waveland, Diamondhead and Pass Christian. These are limited in number to maximize visibility. Email us now to become a Shoofly Partner!

























 RSS Feed
RSS Feed